
What are varicose veins and how does it manifest itself? What happens if you do not treat varicose veins and how to prevent it? We talk about varicose vein complications, explain in detail why trophic ulcers appear and why compression stockings are needed.
What are varicose veins and how does it manifest itself?
The veins have special valves that prevent blood from flowing down the ducts. But with varicose veins, these valves don’t close completely - blood collects in the veins and stretches them.
Symptoms of varicose veins in the early stages:
- The veins on the legs become brighter, more visible;
- On the inner surfaces of the legs and thighs, varicose nodes begin to appear;
- If you stand, sit or walk for a long time, there is a feeling of heaviness in the legs, a feeling of fullness (most often in the evening, in the calves);
- At the place of expansion of the veins, aches or sharp pains appear, in the evening and at night - cramps in the calf muscles;
- The feet were very swollen at the end of the day, but in the morning the swelling disappeared.
Important!
Already at this stage it is necessary to consult a doctor.
With development, varicose veins become chronic (chronic venous insufficiency). symptoms:
- Very winding dark blue intradermal veins appear: they protrude above the surface of the feet and legs, they look like bunches of overripe red grapes;
- There is arching pain in the legs and calves, a feeling of heat in the legs, night cramps in the calf muscles, severe swelling;
- The skin becomes dry, pigmentation appears, it becomes darker, brown spots appear.
Important!
Don't start a disease! With varicose veins, tissue nutrition is disrupted. There is not enough nutrition for the ducts and skin - wounds, eczema and even ulcers appear, which heal very poorly.
Treatment of varicose veins
There are two ways to treat varicose veins: conservative and surgical.
- Conservative: compression therapy. Compression underwear squeezes the affected leg - the diameter of the superficial vein is reduced, the correct pressure in the vein is restored. Blood return decreases, the vessel wall remains in good condition, the valve is closed, the blood does not stagnate and circulates well, the speed of movement of blood through the deep veins increases. The amount of stagnant blood decreases, lymph outflow improves.
- In further cases, when conservative treatment does not help, the doctor will recommend a surgical route: the varicose nodes are removed, the affected veins are removed. To restore function, shunts are placed or valve mobility restored so that the leaflet is closed.
Compression knitwear for varicose veins and ulcers
Compression stockings are special stockings that fit the bottom of the foot and become looser as it rises to the thigh. This improves blood circulation and stimulates blood flow from the bottom of the legs to the heart.
Compression stockings are selected individually, so consult in advance with a phlebologist: you can not choose stockings yourself.
The phlebologist will look at the tone of the veins, where certain valves have problems with not closing the valve. The problem may be, for example, in the thighs: then you need to wear compression stockings. If there is a problem with closing the valve below the knee, then socks or stockings are chosen.
Important!
For maximum effectiveness, compression stockings should be worn at all times - only removed at bedtime.
How to Wear Compression Stockings?
- After getting up, place your feet on the wall and lie down like this for a while - so that the blood flows to the hips as much as possible;
- Without getting up, wear compression stockings.
In this position (lying down, legs raised), blood flow is even, blood does not stagnate. When the compression stockings are in the leg, the veins are in good condition, and the valves are well closed and push blood further through the ducts.
What happens if varicose veins are not treated?
If you do not start varicose vein treatment in time, life -threatening complications may occur:
Thrombophlebitis- inflammation of the veins due to the formation of blood clots in them. symptoms:
- redness;
- the place where the thrombus is located becomes hot;
- inflamed veins are very painful.
If timely treatment is started, the thrombus will stop growing. Residual blood clots can heal for a long time-sometimes months. If left untreated or done incorrectly, clots can grow.
Pulmonary embolism.Thrombuses that appear with thrombophlebitis detach from the walls of the ducts in the legs and come out along with the bloodstream. It clogs the pulmonary artery or its branches - this is fatal. Unfortunately, despite having suspected this complication in a timely manner, doctors were unable to do anything about it.
symptoms:
- chest ache;
- heartbeat accelerated;
- difficulty breathing;
- unreasonable anxiety and unreasonable fear.
Deep vein thrombosis in the lower leg. This is a serious and dangerous complication of varicose veins. The internal veins are clogged, because of this, the outflow of blood almost stops completely - all the tissues of the legs do not receive nutrients and it turns blue.
Venous gangrene in the legs- severe deep vein thrombosis, in which there is no nutrition of the limbs, arterial blood flow is disrupted. Due to the fact that the blood does not flow, gangrene is formed: the feet, in fact, die - starting with the fingers.
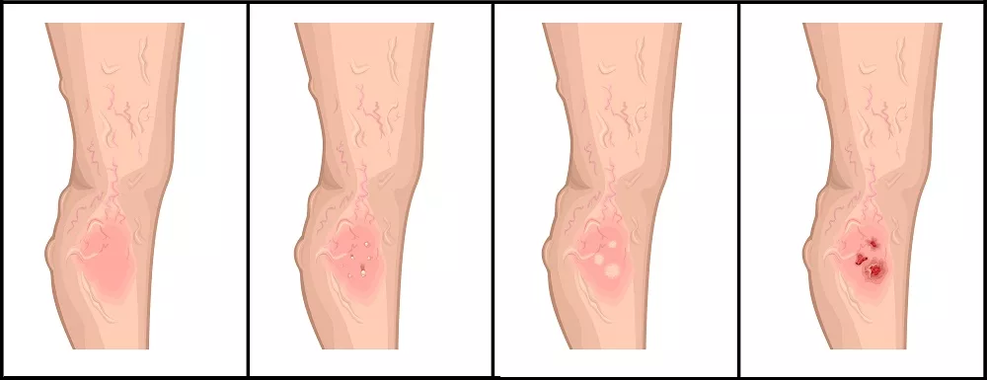
Trophic ulcers- long -term non -healing ulcers that occur due to lack of nutrients in the tissues. Lymph stagnates in the lymphatic vessels, they are under great load and cannot accommodate the amount of lymph. Thus, lymph droplets begin to protrude through the skin. Because of this, the epidermis begins to peel off - ulcers form with dense, ragged edges. Any touch on it causes severe pain.
Bacteria quickly grow in ulcers: the infection merges, the bleeding ulcers begin to purulent. This can lead to very serious complications, including blood poisoning.
Trophic ulcers are of two types:
- veins, when the subcutaneous veins and in the limbs are affected;
- arteries, when the arteries in the legs are affected and the natural nutrition of the limbs is disturbed.
Treatment of trophic ulcers
Trophic ulcers are treated with elastic compression, medications, physiotherapy and surgery.
Trophic ulcer care includes four stages.
The first level - antiseptic
- Antiseptic solution for wound treatment. It is applied on the surface of trophic ulcers, if a cavity has formed under the skin, it is also filled with gel.
- The gel, which has antimicrobial and anti-inflammatory effects, improves microcirculation, reduces redness and swelling of the skin, reduces pain, relieves itching and peeling of the skin, prevents the spread of infection and prevents scarring.
- Aqueous solutions of halogen or benzildimethyl-myristoylamino-propylammonium group antiseptics.
The second stage - a gel to soften dead tissue
Dead tissue is necrosis: black tissue hardens on the surface of the ulcer. If not removed, the ulcer will not heal. To do this, the necrosis is first softened. This is done using a special gel.
The third stage is the formation of an optimal environment for wound healing
Healing is facilitated by the creation of a moist environment inside the wound. If there is no necrosis, use a bandage for quick healing. Here are some suitable bandages:
Alginate bandages:
- Alginate dressings that turn into a soft gel when exposed to wound secretions, provide optimal conditions for moist wound healing;
- A bandage that fills the wound cavity and creates a micro environment that promotes rapid healing;
- Sponge wrap with a layer of hydrogel. Its structure absorbs secretions and maintains a moist environment in the wound;
- Alginate sponge dressing consisting of calcium alginate and hydrocolloids;
- Self -absorbable sterile coating based on sodium alginate, which is ideal for wounds and burns, accelerates healing;
- Hydroactive bandages for deep wounds. Cleans the wound, speeds up its healing, maintains an optimal environment in the wound for up to three days without changing the bandage.
Sponge wrap:
- Double -sided foam bandage. It protects the wound, absorbs discharge from the wound, creates an optimal water balance in the wound;
- Hydrophilic polyurethane sponge wrap;
- Bandages with enzyme and chitosan complexes are suitable for infected wounds (if there is pus in the wound);
- Antimicrobial sponge breathable wrap consisting of a polyurethane layer of sponge and a silver alginate matrix.
The fourth stage - wound healing
Once the wound has been cleaned and an optimal environment has formed in it, it begins to heal, the edges of the wound shrink. For safe and fast healing, use a special bandage.
Mesh ointment bandage:
- Ointment bandage with Peruvian balm to use when fresh skin appears on the wound;
- Ointment bandages based on triglycerides, which promote healing and care for wound edges;
- The bandage looks like a waxy rectangle, soft and quite dense. Can be on the wound for up to seven days;
Film bandages that can be used to repair bandages on wounds:
- Waterproof film bandage (but breathable), protects the wound from microorganisms. It can be used to repair previous bandages and as an independent bandage.
- Transparent film polyurethane bandage, the skin under it does not sweat, breathable.
Important!
This bandage is ideal for healing not only trophic ulcers, but also any wounds that have long healed.
Prevention of varicose veins
- Move as much as possible: the more you move, the better the blood circulates in the veins;
- Get rid of bad habits;
- Contact a phlebologist in a timely manner at the first symptoms of the disease;
- Periodically perform an ultrasound on the vessel - the doctor will notice the changes first;
- After a day of work, go home and lie with your feet against the wall for about 15 minutes.
Prevention of trophic ulcers
- Watch your weight: it puts pressure on your legs, loading the vascular and lymphatic systems. If necessary, follow a diet;
- Walk as often as possible;
- If possible, lift your legs, place your feet in a high position as often as possible. In the evening, you can lie on the couch and lift your legs, placing them on the wall: you need to lie down like this for at least 15 minutes;
- Treat the lower veins in time;
- Quit smoking - it greatly reduces the blood supply to tissues and contributes to the development of trophic ulcers;
- Take care of your feet: wear appropriate shoes so that they do not sting or rub;
- Check your feet regularly: check the color of the skin on your feet. If the feet turn blue in the evening and veins appear on the feet, contact a phlebologist;
- Moisturize the skin with a softening, moisturizing, nourishing cream;
- Keep your feet warm, dressed for the weather;
- Try not to injure the skin.


















